
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
Original Articles
- Cardiovascular Risk/Epidemiology
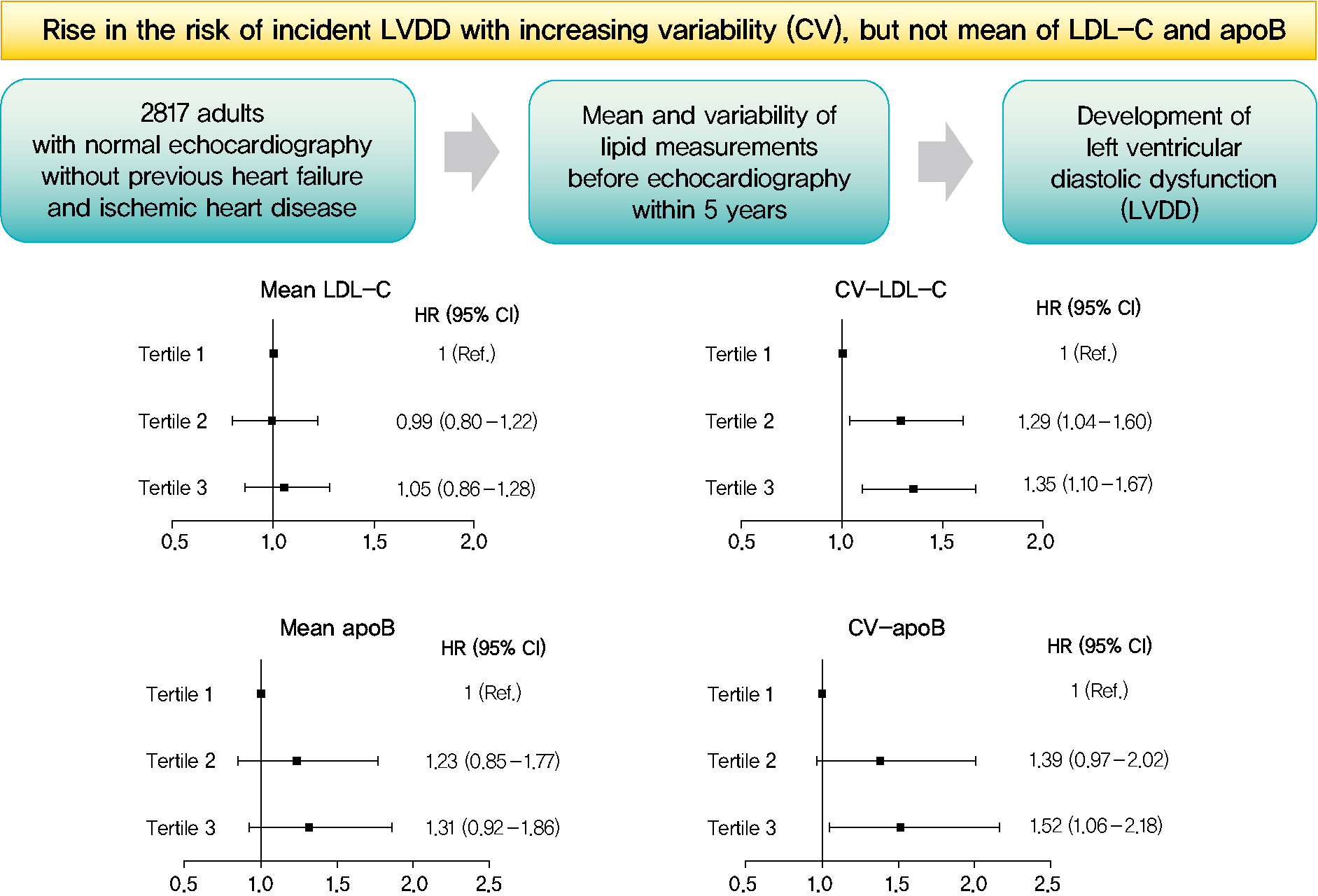
- Mean and Variability of Lipid Measurements and Risk for Development of Subclinical Left Ventricular Diastolic Dysfunction
- Jiyun Park, Mira Kang, Jiyeon Ahn, Min Young Kim, Min Sun Choi, You-Bin Lee, Gyuri Kim, Kyu Yeon Hur, Jae Hyeon Kim, Jeong Hoon Yang, Sang-Man Jin
- Diabetes Metab J. 2022;46(2):286-296. Published online November 22, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0080
- 5,692 View
- 196 Download
- 1 Web of Science
- 2 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 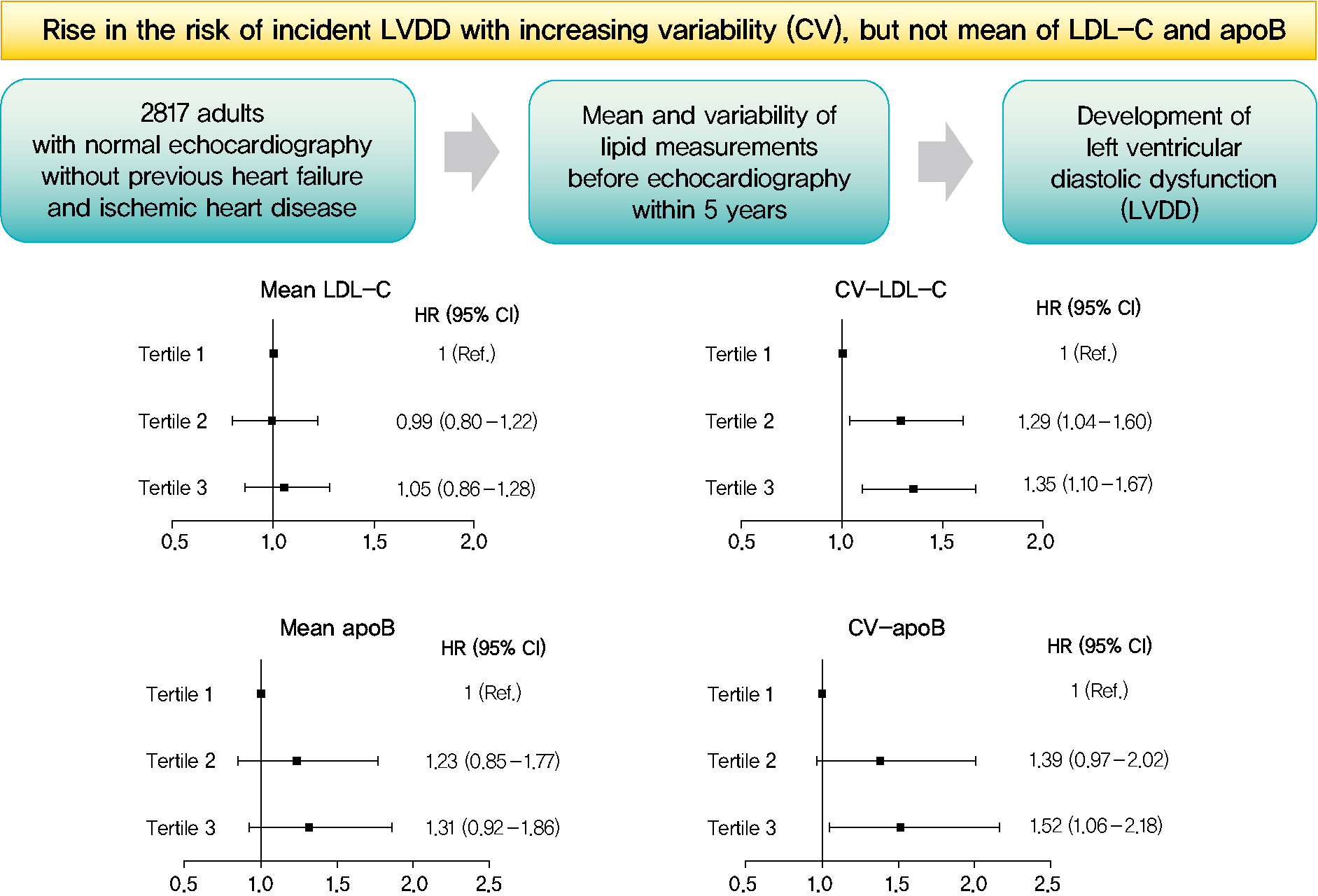
- Background
Subclinical left ventricular diastolic dysfunction (LVDD) is an emerging consequence of increased insulin resistance, and dyslipidemia is one of the few correctable risk factors of LVDD. This study evaluated the role of mean and visit-to-visit variability of lipid measurements in risk of LVDD in a healthy population.
Methods
This was a 3.7-year (interquartile range, 2.1 to 4.9) longitudinal cohort study including 2,817 adults (median age 55 years) with left ventricular ejection fraction >50% who underwent an annual or biannual health screening between January 2008 and July 2016. The mean, standard deviation (SD), coefficient of variation (CV), variability independent of the mean (VIM), and average real variability of total cholesterol, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), apolipoprotein B (apoB), non-HDL-C, and triglycerides were obtained from three to six measurements during the 5 years preceding the first echocardiogram.
Results
Among the 2,817 patients, 560 (19.9%) developed LVDD. The mean of no component of lipid measurements was associated with risk of LVDD. CV (hazard ratio [HR], 1.35; 95% confidence interval [CI], 1.10 to 1.67), SD (HR, 1.27; 95% CI, 1.03 to 1.57), and VIM (HR, 1.26; 95% CI, 1.03 to 1.55) of LDL-C and all the variability parameters of apoB were significantly associated with development of LVDD. The association between CV-LDL and risk of LVDD did not have significant interaction with sex, increasing/decreasing trend at baseline, or use of stain and/or lipid-modifying agents.
Conclusion
The variability of LDL-C and apoB, rather than their mean, was associated with risk for LVDD. -
Citations
Citations to this article as recorded by- Separate and Joint Associations of Remnant Cholesterol Accumulation and Variability With Carotid Atherosclerosis: A Prospective Cohort Study
Jinqi Wang, Rui Jin, Xiaohan Jin, Zhiyuan Wu, Haiping Zhang, Ze Han, Zongkai Xu, Yueruijing Liu, Xiaoyu Zhao, Xiuhua Guo, Lixin Tao
Journal of the American Heart Association.2023;[Epub] CrossRef - Variability of Metabolic Risk Factors: Causative Factor or Epiphenomenon?
Hye Jin Yoo
Diabetes & Metabolism Journal.2022; 46(2): 257. CrossRef
- Separate and Joint Associations of Remnant Cholesterol Accumulation and Variability With Carotid Atherosclerosis: A Prospective Cohort Study
- Effects of Islet Transplantation on Endogenous beta-cell Regeneration after Partial Pancreatectomy in Rodents.
- Hye Seung Jung, You Ran Ahn, Seung Hoon Oh, Jung Hwa Jung, Tae Hyun Kim, You Cheol Hwang, Mira Kang, Yongsuk Bae, Young seok Kim, Jae Hoon Chung, Yong Ki Min, Myung Shik Lee, Moon Kyu Lee, Kwang Won Kim
- Korean Diabetes J. 2007;31(2):113-122. Published online March 1, 2007
- DOI: https://doi.org/10.4093/jkda.2007.31.2.113
- 2,240 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Islet transplantation is one of regimens supplying the deficient insulin in diabetes patients, but the effects of islet grafts on the changes of endogenous beta-cells are not clear. In the present study, we examined the changes of endogenous beta-cell mass after islet transplantation in partially pancreatectomized mice. METHODS: Balb/c mice were 70% pancreatectomized, transplanted with syngeneic islets (group IV), and were compared with pancreatectomized mice treated with insulin (group III) or no insulin (group II). Blood glucose levels and body weight were monitored. Remnant pancreas was obtained at 6 or 10 days after pancreatectomy, and immunohistochemical staining was done for the evaluation of beta-cell mass changes. RESULTS: Hyperglycemia and weight loss were induced after pancreatectomy. After islet transplantation or insulin treatment, blood glucose levels recovered to normal, and body weight started to increase. Plasma insulin levels were higher and beta-cell mass was larger in group IV than in group II (P < 0.05). Especially, the difference of beta-cell mass between them was more evident at 7 days as compared to at 3 day after transplantation. When compared to group III, group IV showed larger individual beta-cell area after 7 days and larger beta-cell mass after 3 days of islet transplantation (P < 0.05). CONCLUSION: These observations indicate that islet transplantation plays a role in enhancing remnant beta-cell regeneration after partial pancreatectomy in rodents.
- Maximal Oxygen Uptake (VO2max) and Metabolic Syndrome.
- Mira Kang, Ji Dong Sung, Byung Chul Yoo, Yoon Ho Choi, Sae Young Jae, Jae Hoon Chung, Yong Ki Min, Myung Shik Lee, Kwang Won Kim, Moon Kyu Lee
- Korean Diabetes J. 2005;29(1):65-71. Published online January 1, 2005
- 1,167 View
- 23 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
A number of studies have demonstrated an inverse relationship between cardiorespiratory fitness and metabolic syndrome. However, whether the maximal oxygen uptake (VO2max) is dependent on the number of metabolic components or on particular metabolic component remains to be assessed. METHODS: A total of 1,432 Korean subjects were studied. Each individual was assessed for the presence of metabolic syndrome using the modified NCEP-ATP III criteria. All subjects underwent a graded symptom-limited maximal exercise test to determine their VO2max, using a treadmill according to the Bruce protocol. RESULTS: The age-adjusted prevalence of metabolic syndrome in all subjects was 20.4%. The odds ratios for metabolic syndrome were higher in men, the elderly, the obese and those with a lower VO2max. The difference in the VO2max was dependent only on the presence of metabolic syndrome, not on the number of components. CONCLUSION: There were no significant differences in the VO2max according to the presence of particular metabolic components. These results suggest that the VO2max reflects the metabolic syndrome state, rather than the metabolic components, and might be a factor in determining metabolic syndrome

 KDA
KDA
 First
First Prev
Prev





